Seattle Children’s Sickle Cell Program Makes Significant Progress Toward Becoming a Center of Excellence
February 7, 2024
Over the past 18 months, members of the Seattle Children’s Sickle Cell Disease Program have continued working diligently to improve and enhance care for children, teens and young adults with sickle cell disease (SCD) by expanding services, hours, and staffing, with a special focus on hiring a diverse team that represents the nearly 150 patients and their families we serve in the Pacific Northwest.
For more than two decades, Seattle Children’s and Odessa Brown Children’s Clinic (OBCC) has treated patients with SCD and we aim to be a medical home and center of excellence in which all families feel empowered, welcomed, and well cared for. As part of our ongoing program enhancements, we are launching a new program in January 2024 that pairs every patient with sickle cell disease with an equity-focused social worker when visiting Seattle Children’s Emergency Department (ED) or staying overnight at the hospital. The social worker will ensure patient families have the resources and support they need during their stay.
About SCD
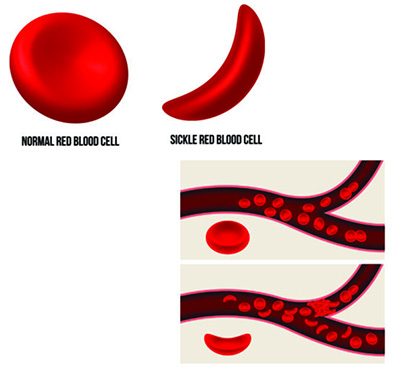
SCD is a group of blood conditions that affect hemoglobin, a key protein in red blood cells that delivers oxygen to cells in the body. In patients with SCD, this hemoglobin protein does not work correctly and can twist the red blood cell into a “sickled” shape, reducing oxygen delivery and causing pain. In the United States, about 100,000 Americans are affected by SCD, most of whom are of African or Hispanic heritage. The disease can affect anyone, however, including people of southern European, Middle Eastern or Asian Indian heritage.
People with SCD deal with unique and complex issues, often requiring visits with multiple medical specialists. To meet the needs of our patients and reduce multiple appointments for families, we introduced a multidisciplinary care team approach and expanded provider visits from 1.5 days a week to five days a week between our two locations — OBCC Othello and Seattle Children’s hospital campus.
Addressing the Risk of Stroke
When the red blood cells change shape, they can get stuck in the brain, prevent the delivery of oxygen and potentially cause a stroke.
A transcranial doppler (TCD) ultrasound uses sound waves to measure how fast blood is flowing to the brain to determine a child’s risk of stroke. We installed a TCD ultrasound machine at OBCC Othello in September 2022, which means kids with SCD who need a TCD ultrasound as part of their routine care can get everything done in one visit instead of traveling to a separate facility.
Neurocognitive Screenings
Dr. Sandy Rodgin is the new neuropsychologist on the SCD team. She conducts regular neurocognitive screenings to help recognize when a child with SCD also has cognitive issues that may impact their reasoning skills, judgment, memory and learning.
“Children with sickle cell disease have an increased chance of having difficulties with attention and focus, as well as executive functioning skills,” she said. “They also are at increased risk for having delays in speech and language milestones when they’re younger. These difficulties have been found even when there aren’t differences shown on brain imaging studies.”
Dr. Rodgin works with the child’s medical providers to develop a plan that addresses potential issues. She also puts together educational plans with the child’s school to ensure they receive appropriate accommodations.
New Care Team Members
In addition to Rodgin, Seattle Children’s Sickle Cell Disease Program also recently welcomed:
- Kristine Karvonen, a pediatric hematologist and oncologist who has a specific interest in SCD and racial and ethnic health disparities.
- Beth Willard, a nurse practitioner who cares for patients at Seattle Children’s hospital campus.
- Lauren Frazier, a social worker dedicated to helping patients with SCD and their families find social, financial and community resources.
- Kathryn Querin, a Child Life specialist who works with children to help them relieve tension, express concerns and fears, and feel more in control about their medical experience.
SCD Program’s Commitment to Equity
As part of our ongoing work to be an anti-racist organization and uphold our core value of equity through Seattle Children’s Health Equity and Anti-Racism Action Plan, we formed the Sickle Cell Disease External Advisory Board (EAB) in May 2022 to gather feedback and ideas on how to improve the care and services we provide within Seattle Children’s Sickle Cell Disease Program.
In early 2023, the EAB determined that both Seattle Children’s hospital campus and OBCC had made significant progress toward improving and growing the SCD program to deliver optimal and respectful medical care for patients with SCD and their families. However, they also shared that there is still more work to do to better improve the patient and family hospital experience.
To address that need, Seattle Children’s Center for Diversity and Health Equity will launch a pilot program in January 2024 where consultants visit patients with SCD who come to Seattle Children’s Emergency Department for care or are staying at the hospital. The consultants are experienced care team members with expertise in health equity and anti-racist interventions, who will ask about a family’s experiences at Seattle Children’s and identify any areas where they may need additional resources and support. In some instances, this may include addressing issues related to equity. The consultants will be available during regular business hours, Monday through Friday from 8 a.m. to 5:30 p.m., and will build a process for connecting with families who present for care outside of business hours.
“Through this new program, we hope families benefit from the additional advocacy and support as close to the point of care as possible and will feel like we are taking their concerns seriously by actively addressing the problems the first time they raise an issue,” said Maya Scott, director of Seattle Children’s Center for Diversity and Health Equity.
Looking Ahead
Looking ahead, some of our next efforts will focus on developing a clinic with UW Medicine that better supports teens with SCD as they transition to adult care.
We also have plans to offer Pulmonary and Sleep Medicine services soon to help patients with SCD who have trouble breathing or difficulty sleeping.
Dr. Shaquita Bell and Dr. Mignon Loh co-lead the Seattle Children’s Sickle Cell Disease Program. Bell is senior medical director of OBCC and Loh serves as division head for Hematology, Oncology, Bone Marrow Transplant and Cellular Therapies at Seattle Children’s. They feel optimistic about the program’s progress and are committed to the continued growth to help advance the care of children, teens and young adults with SCD..
“Our goal through the Sickle Cell Disease Program is to make it easier and more convenient for patients and their families to access all the different types of care they need, and for our staff to deliver equitable care with compassion,” said Dr. Loh.