Finding an Allergy Brake
 May 16, 2023 – Researchers in the Center for Immunity and Immunotherapies at Seattle Children’s Research Institute and colleagues have discovered a new mechanism in human mast cells: They express an inhibitory receptor called Siglec-9 that can act as a brake on their activation.
May 16, 2023 – Researchers in the Center for Immunity and Immunotherapies at Seattle Children’s Research Institute and colleagues have discovered a new mechanism in human mast cells: They express an inhibitory receptor called Siglec-9 that can act as a brake on their activation.
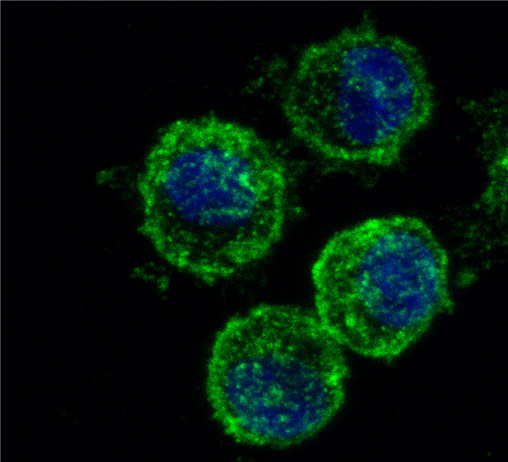
Mast cells are found in tissues throughout the body — particularly on skin and in the respiratory and digestive tracts — as part of the immune system. They provide a line of defense against disease; in response to exposure to germs, viruses and parasites, mast cells set off a rapid inflammatory response. But mast cells also play a prominent role in the activation of allergies, when the cells respond to harmless triggers as if they were a threat.
The findings, recently published in the Journal of Allergy and Clinical Immunology, looked at Sialic acid–binding immunoglobin-like lectins (Siglecs), cell surface receptors predominantly found on immune cells. The researchers used gene-editing techniques to determine their expression and function in human mast cells.
Siglec-9 expression and function in mast cells had been largely unexplored. Studies of its role in other cells focused on its detrimental effects, including dampening immune response to certain pathogens and impairing immune surveillance in some cancers. But other recent studies support the use of Siglec-9 to inhibit excessive immune cell activation and limit the magnitude of the inflammatory response in arthritis, colitis and severe coronavirus disease.
Dr. Adrian Piliponsky, principal investigator at the research institute and an assistant professor in the departments of departments of Pediatrics, Pathology, and Global Health at the University of Washington School of Medicine, oversaw the study and said it demonstrates that Siglec-9 interactions with Siglec-9 ligands (cellular signaling begins with the binding of a signaling molecule, or ligand, to its receiving molecule, called a receptor) or anti-Siglec-9 antibodies can limit the ability of mast cells to undergo activation by mechanisms that mimic mast cell activation during allergic disease.
Piliponsky said his team’s research may lead to the design of new therapeutics to treat mast cell-associated disorders such as mastocytosis (a rare disorder that results in excess mast cells building up in the body), chronic urticaria (long-term hives) and allergic disease.
“Studies are on their way in our lab to address the impact of Siglec-9 inhibitory effects on mast cell function in pre-clinical models of mast cell-associated disease,” Piliponsky said. “Long-term goals for our research include the design of therapeutics targeting Siglec-9 in mast cells to prevent allergic disease.”
The research team believes further understanding of Siglec-9’s contribution to mast function in both normal conditions and in disease may be needed to tailor potential Siglec-targeted therapies for treatment of mast cell-associated disorders.
Study contributors include lead author Dr. Irina Miralda (postdoctoral fellow) and Dr. Nyssa Samanas, Albert Seo, Jake Foronda and Josie Sachen, all of the Piliponsky Lab; Dr. Shane Morrison, plastic surgeon in Seattle Children’s Craniofacial Center and assistant professor of Plastic Surgery at the University of Washington School of Medicine; and researchers from the University of South Carolina School of Medicine.
The study was supported with seed funding from the research institute and National Institutes of Health/National Institute of General Medical Sciences pilot project funding. Lung tissue was procured through the National Disease Research Interchange program with support from the National Institutes of Health.
— Colleen Steelquist
