New Criteria for Pediatric Sepsis Identified
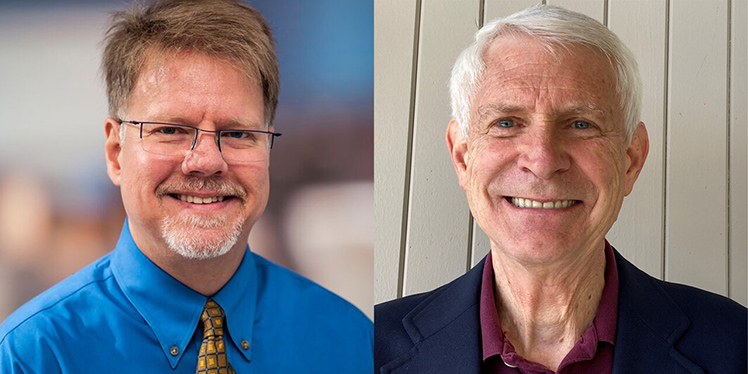 Jan. 22, 2024 – Researchers at Seattle Children’s Research Institute have identified new criteria for defining pediatric sepsis and septic shock that can be applied across health institutions globally. The latest criteria, published in JAMA and authored by Dr. Scott Watson in the Center for Child Health, Behavior and Development and Dr. Jerry Zimmerman in the Center for Clinical and Translational Research, in collaboration with international experts in pediatric sepsis, will update current sepsis criteria, which, until recently, excluded clear definitions of sepsis in children. Coinciding with the publication, the new criteria were announced on Jan. 21 at the Society of Critical Care Medicine's 2024 Critical Care Congress in Phoenix, Arizona.
Jan. 22, 2024 – Researchers at Seattle Children’s Research Institute have identified new criteria for defining pediatric sepsis and septic shock that can be applied across health institutions globally. The latest criteria, published in JAMA and authored by Dr. Scott Watson in the Center for Child Health, Behavior and Development and Dr. Jerry Zimmerman in the Center for Clinical and Translational Research, in collaboration with international experts in pediatric sepsis, will update current sepsis criteria, which, until recently, excluded clear definitions of sepsis in children. Coinciding with the publication, the new criteria were announced on Jan. 21 at the Society of Critical Care Medicine's 2024 Critical Care Congress in Phoenix, Arizona.
Sepsis is a life-threatening condition, caused by a dysregulated inflammatory response in the body due to a wide range of bacterial, viral or other types of infections. If left untreated, sepsis can evolve into tissue damage, major organ failure and death. The onset of sepsis is acute and is one of the leading causes of death among children worldwide.
Despite the acuity of this condition, there is currently no single test to identify sepsis. Typically, healthcare providers use a series of tests to identify infection and organ dysfunction to help inform a diagnosis. Due to time or resource constraints, this process could present barriers for timely treatment.
The previous criteria to identify pediatric sepsis were published in 2005 by the International Pediatric Sepsis Consensus Conference and have since been adapted to facilitate a wide range of clinical, research, quality and policy improvement efforts. These criteria, based on expert opinion, defined sepsis as suspected or confirmed infection in the presence of a systematic inflammatory response syndrome.
In 2016, the Third International Consensus Conference for Sepsis and Septic Shock (Sepsis-3) revised sepsis criteria in adults, collating a wide range of data from patients with suspected infection in the United States and Germany. While this was helpful to inform overall sepsis treatment, sepsis can present very differently in children and thus, Sepsis-3 guidelines did not include information validated in children with sepsis.
The Society of Critical Care Medicine assembled a collaborative task force of 35 pediatric experts from six different countries with knowledge of critical care, emergency medicine, infectious disease, nursing and general pediatrics to inform these new criteria. This research group reviewed international data based on more than 3 million hospital encounters in the U.S. and globally, and from four lower-resource settings. Seattle Children’s was one of the sites contributing data to this effort.
This study resulted in updated recommendations defining sepsis in children, using a novel scoring matrix known as the Phoenix Sepsis Score. Children that score 2 or higher on the Phoenix Sepsis Score have potentially life-threatening organ dysfunction and a diagnosis of sepsis and require urgent, vigilant care. Consistent presentation of these signs of organ dysfunction across multiple global sites supports the feasibility of implementing these criteria into global practice. Currently, the Centers for Disease Control and Prevention is developing a national surveillance system for sepsis in hospitalized children based on the Phoenix Sepsis Score.
“These criteria provide, for the first time, an objective, data-driven way to identify life-threatening organ dysfunction in children caused by infection,” Watson said. “This work aims to open up a path for better care for children with severe infections.”
This research was funded by the Society of Critical Care Medicine and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Read the full investigation on JAMA, and accompanying publication.
— Empress Rivera-Ruiz
