Terri Laguna, MD, MSc, a pediatric pulmonologist, did not expect to find herself back at Seattle Children’s some 20 years after completing her medical training there. “To be completely straightforward,” she says, “I would not have accepted the job and returned to Seattle Children’s if there was not going to be this center focused on respiratory biology.”
Laguna refers to the Center for Respiratory Biology and Therapeutics (CRBT), part of Seattle Children’s Research Institute. Launched in October 2023, it aims to build on Seattle Children’s distinguished legacy of innovations in the treatment of cystic fibrosis (CF) and broaden its impact to encompass a wider array of respiratory disorders.
Leading this ambitious initiative are some of the field’s leading researchers and clinicians. Their collective expertise, inventive approaches and dedication to collaborative efforts are poised to make significant strides in tackling complex respiratory challenges.
For Laguna, now serving as the division head of pulmonary and sleep medicine at Seattle Children’s, the new team and the research opportunities presented at the center were a “huge draw” — heralding a “period of rejuvenation”, she says, for her scholarly pursuits. Laguna is focused on better defining infection and inflammation in the CF airway and championing diversity, equity and inclusion in the pediatric pulmonary workforce.
“There has been a palpable enthusiasm around the work that is ongoing and the potential opportunities within CRBT,” she says. “It’s just incredibly exciting.”
Bridging divides
 A therapeutic surfactant aerosol — an inhaled treatment for premature infants — is being developed in collaboration with Virginia Commonwealth University researchers and tested in the Center for Respiratory Biology and Therapeutics’ DiBlasi Lab. Credit: Michael Hindle
A therapeutic surfactant aerosol — an inhaled treatment for premature infants — is being developed in collaboration with Virginia Commonwealth University researchers and tested in the Center for Respiratory Biology and Therapeutics’ DiBlasi Lab. Credit: Michael HindleIn addition to advancing new therapies for diseases ranging from asthma and pulmonary hypertension to sleep-disordered breathing and progressive lung-scarring disorders, the new center is home to technology development focused on inhaled drug delivery systems and innovative respiratory support mechanisms.
What is more, CRBT takes on respiratory health equity research and is implementing quality improvement initiatives to ensure that the benefits of its discoveries and treatments are accessible to all segments of the population.
Much of this work was already happening at Seattle Children’s, but it was scattered across different locations between investigators who would rarely interact. Clinical efforts would take place at the hospital campus nestled in a northeastern Seattle neighborhood, while the thrust of basic research unfolded in labs closer to the city center.
This physical separation often posed challenges to seamless collaboration and integration of findings from bench to bedside, says Jason Debley, MD, MPH, a pediatric pulmonologist serving as interim director of CRBT. By bridging these divides, the center aims to foster a more cohesive environment where clinicians and basic scientists from a vast array of disciplines, including community health, global health, pediatric pulmonary, sleep medicine, otolaryngology, critical care, neonatology, pathology and respiratory therapy, can work in close partnership, facilitating the rapid translation of research discoveries into tangible healthcare improvements.
“We’re uniting these investigators with a shared purpose,” says Debley, “and the sum is much greater than its parts. Virtually overnight, we’ve managed to bring together a diverse range of cross-disciplinary expertise, all under a single umbrella.”
In the realm of possibility
The CRBT taps into Seattle Children’s long history of developing treatments for CF. For more than 25 years, the hospital has stood as the cornerstone of a national CF research network, coordinating more than 150 multi-center therapeutic trials and providing clinical, statistical, data management and regulatory expertise to help make these studies happen.
This undertaking not only facilitated the approval of groundbreaking CF drugs — treatments that helped to transform a once deadly lung disorder into a manageable condition for most patients — but also pioneered innovative clinical trial designs and statistical methods, showcasing the power of collaboration among dedicated respiratory researchers.
“CF is this fantastic example of what is possible,” says Debley. Through CRBT, he and his colleagues now hope to replicate that success, and build upon it, across all areas of pediatric respiratory medicine.
In the treatment of primary ciliary dyskinesia (PCD), for example, pulmonologists Drs. BreAnna Kinghorn and Margaret Rosenfeld are exploring innovative trial protocols that could help bring new therapies to fruition for this rare genetic lung disorder, in which tiny hair-like structures along the airways do not beat properly, leading to mucus buildup and persistent infections.
Drawing inspiration from CF research successes at Seattle Children’s, Rosenfeld and her CRBT colleagues are testing the feasibility of using mobile health monitoring and home measurement tools to enable decentralized study designs, a possible solution to the challenge of studying rare diseases in small patient groups.
Catalyzing discoveries
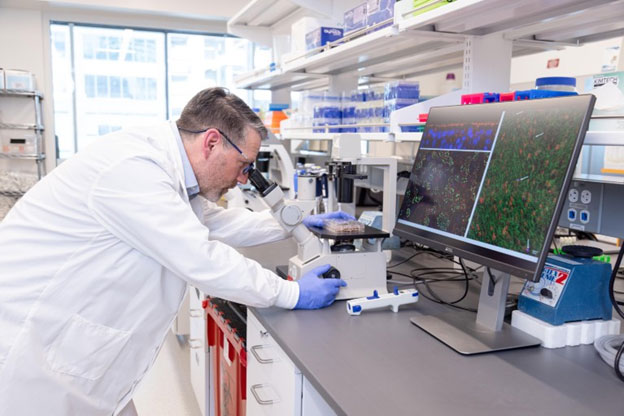
Seattle Children’s Jason Debley, a pediatric pulmonologist and the interim director of the Center for Respiratory Biology and Therapeutics, observes airway epithelial cells from his lab’s large biorepository under microscopy. Credit: Seattle Children’s
Others at CRBT are delving into the mechanistic underpinnings of how a range of congenital and acquired structural airway abnormalities cause severe airway disease, with each interconnected line of inquiry intended to promote a cyclical research process that moves from patient care to laboratory analysis and back again.
“That’s the kind of thing that’s really exciting,” says pulmonologist Christopher Goss, MD, a CF specialist who serves as associate dean for clinical research across the entire University of Washington School of Medicine system. Goss especially values CRBT’s regular seminars and other events where researchers across Seattle Children’s various sites come together to learn, interact and share ideas. Investigators then have the opportunity to apply for internal grant funding to get outside-the-box project ideas off the ground.
“Bringing these disparate parties together will really catalyze new discoveries,” Goss says.
Debley is leading by example in this regard. His own research has long focused on the role of airway epithelial cells in childhood asthma. And, over the past 15 years, he has built a large repository of patient samples collected by a specialized ‘brushing’ technique from the lower airways of both asthmatic and healthy children, each characterized with detailed medical histories.
In the lab, Debley’s team converts the cells into three-dimensional (3D) models that mimic human airways to study how these organ-like epithelial cultures react to viruses and allergens and interact with immune and airway structural cells. Leveraging comprehensive molecular techniques — including bulk and single-cell transcriptomics, proteomics and epigenomics — they have begun to tease apart how such responses influence immune regulation. Debley’s goal, he explains, is “to identify novel disease mechanisms and therapeutic targets in asthma”.
Model of success
CRBT investigators are spearheading similar bedside-to-bench-and-back-again strategies in their examinations of congenital airway abnormalities, lung diseases of prematurity and other pediatric respiratory conditions — with a major focus on the development of cell culture models built using tissue samples taken from children with and without airway disease.
In their research into bronchopulmonary dysplasia — a chronic lung disease that impacts newborns — a team led by pulmonologist Laurie Eldredge, MD, PhD and pathologist Gail Deutsch, MD is collecting lung tissue from infants born early with underdeveloped airways. The researchers then build organ-like structures and use small-animal models to deepen their understanding of the disease’s mechanisms and to identify biomarkers that can help clinicians determine which preterm infants face the highest risk of severe lung complications.
These efforts are setting the stage for clinical trials, scheduled to begin in the coming years, of new cell-based therapies designed to reduce lung damage in these vulnerable infants.
Laboratory models of this kind have also been instrumental for pulmonologist Stephen Reeves, MD, PhD and his colleagues to explore the crosstalk between different cells in the airways and the supporting extracellular matrix. This research has uncovered potential drug targets within the extracellular matrix, offering new avenues for treating airway inflammation and fibrosis in children — including for diseases such as virus-associated bronchiolitis that currently lack targeted therapies.
Other cellular modeling work at CRBT aims to define the signaling processes that underpin structural development in the airways and determine how disruptions in cell communication contribute to congenital diseases such as tracheal stenosis (narrowing of the airpipes) and tracheomalacia (airway collapse during breathing).
'Radical integration'
Venturing beyond the cellular laboratory and into the surgical suite, CRBT also features an innovative program dedicated to personalized surgical planning and device development. This interdisciplinary initiative brings together biophysicists, respiratory therapists, otolaryngologists, lung pathologists and others with a shared philosophy — what Debley calls “radical integration”. Their collective aim is to harness the power of 3D printing and advanced medical imaging to deepen the field’s understanding of lung architecture and flow dynamics. This effort is ultimately geared toward optimizing respirator designs and drug delivery technologies tailored for prenatal airway conditions.
Integrated teams of basic and clinical investigators at CRBT are exploring topics related to sleep-disordered breathing, climate-driven contributors to asthma, respiratory care in resource-limited settings and more. “The new center has really bootstrapped these collaborative research initiatives,” says Debley, anticipating that collaboration will further intensify as CRBT grows, secures additional funding and attracts fresh talent. “We’re pulling all together now with a common mission.”
And just as pulling air into the lungs depends on the coordinated action of a working respiratory system, coordinated efforts from basic, translational and clinical researchers will allow CRBT to breathe new life into cutting-edge respiratory research, facilitating the discovery and development of novel therapeutics for children worldwide.
— Originally published in scientific journal, Nature.
About the Center for Respiratory Biology and Therapeutics
Unifying basic, translational, clinical, epidemiologic and global health research, the physician-scientists at Seattle Children’s Center for Respiratory Biology and Therapeutics are leading transformative “bench to bedside and back” efforts to drive the next phase of discoveries and novel therapeutics for pediatric respiratory diseases. Learn more.
