Strategies for Improving Vaccine Uptake: A Q&A With Drs. Doug Opel and Doug Diekema
Vaccines have played an important role in improving the health of children. However, some parents express concerns about vaccine safety and question the necessity of vaccines, and as a result, vaccine-preventable illnesses such as measles are currently on the rise in the United States. Seattle Children’s physicians Dr. Doug Opel and Dr. Doug Diekema from the Treuman Katz Center for Pediatric Bioethics and Palliative Care recently wrote a clinical report from the American Academy of Pediatrics on strategies for improving communication with families about vaccines. Provider News sat down with them to discuss what pediatricians can do to address parental concerns and improve vaccination rates.
Q. What is vaccine hesitancy and what are common causes?
A. Vaccine hesitancy is a motivational state of being conflicted about, or opposed to, getting vaccinated. Vaccine hesitancy may result in a range of vaccine behaviors. Some vaccine-hesitant parents may refuse all vaccinations. Some may decide to only allow some. And others may, in the end, decide to have their child receive most or all recommended vaccinations, yet they may harbor lingering concerns about vaccines. Those concerns can negatively impact vaccine decision-making at future visits or with subsequent children.
Many factors contribute to vaccine hesitancy. Parent concerns about the safety of vaccines is one particularly prominent factor. Distrust in those who develop vaccines and recommend them is another important factor. Trust in sources that may spread disinformation about vaccines and encourage distrust in physicians, public health officials and government requirements surrounding vaccination is yet another contributor. Ultimately, the causes of vaccine hesitancy are multifactorial, with individual beliefs; group norms and peer influences; social media; and cultural, religious and political beliefs playing a role.
Q. What role do pediatricians play in addressing vaccine hesitancy among their patient families?
A. One of the most important things we can do is remind ourselves how influential we are to a parent’s decision-making about vaccines. Though it doesn’t always feel like it, pediatric clinicians are routinely cited as the most common source of vaccine information for parents and the most trusted source for vaccine-safety information. Research supports that we positively impact a parent's vaccine behavior, even among parents with concerns about vaccines. Reminding ourselves that most parents want to trust us and hear what we have to say about vaccines can help us devote the time and attention needed for these conversations.
Q. What communication strategies can pediatricians use to improve vaccination uptake?
A. With recent advances in our understanding of what constitutes effective vaccine communication, clinicians now have more tools than ever in this toolbox. Two communication strategies in particular are worth noting. First, give parents a strong, high-quality vaccine recommendation. There is higher vaccine receipt among children whose parents receive a very strong clinician vaccine recommendation than those who do not. Second, use a presumptive format to initiate the vaccine recommendation, such as “Sara is due for several vaccines today,” rather than a participatory one, such as “How do you feel about vaccines today?” This simple change in framing sets vaccination as the default, which itself increases vaccine uptake while still allowing for a discussion about any concerns parents may have.
Q. What if a family continues to refuse or delay vaccination?
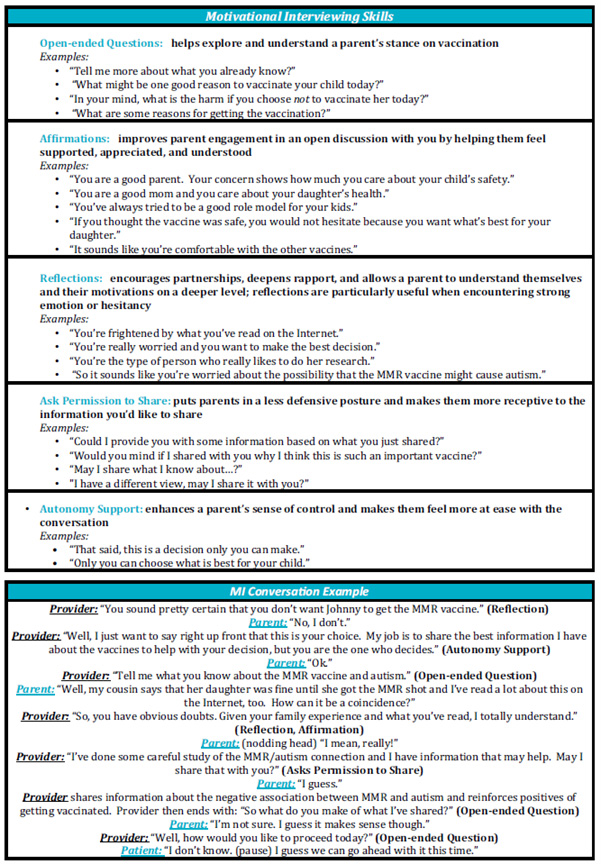
A. Consider using motivational interviewing (see below) to help move parents along toward the desired goal of accepting vaccines. There is some evidence that this technique is effective in the vaccine context, and as a patient- and family-centered framework for behavior change, it can help nurture trust, build partnership and deepen rapport with families regarding vaccination. Showing respect, listening carefully to parent concerns, finding common ground with the parent, and being willing to compromise can all be helpful in strengthening trust and keeping communication open.