Rheumatic Heart Disease
What is rheumatic heart disease?
Rheumatic (pronounced roo-MAT-ik) heart disease is a condition in which rheumatic fever damaged the heart. Typically, this long-term damage happens to the mitral valve, aortic valve or both. This damage may cause a valve to “leak” or become narrow over time.
The mitral valve (between the left atrium and left ventricle) is usually more affected than the aortic valve (between the left ventricle and aorta).
Rheumatic heart disease can be prevented by preventing rheumatic fever.
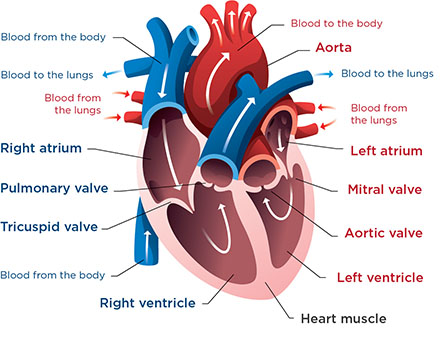
This image shows a normal heart. In some children, rheumatic fever causes lasting damage to the mitral valve or aortic valve. It can also affect the heart muscle (myocardium) or the outer covering around the heart (pericardium).
-
What is rheumatic fever?
Rheumatic fever happens after an infection from bacteria called group A streptococcus if the infection is not completely treated with medicine (antibiotics). Group A streptococcus (strep) is the bacteria that causes strep throat, scarlet fever and other infections. Rheumatic fever causes inflammation and may affect the heart, joints, skin and brain.
Symptoms of rheumatic fever may include:
- Fever
- Joint swelling, tenderness or redness over multiple joints
- Small bumps or nodules under the skin
- Rash
- Weight loss
- Fatigue
- Stomach pain
-
How does rheumatic fever damage the heart?
Rheumatic fever may cause serious, permanent damage to the heart valves. Most often, it damages the mitral valve, aortic valve or both. These valves act like doors in the heart that allow blood to pass between or out of the chambers on the left side of the heart. If rheumatic fever damages the valves:
- They may not be able to open fully. This causes narrowing of the valve (stenosis).
- They may not be able to close fully. This causes a “leak.”
Valve damage from rheumatic fever is known as valvulitis. This means inflammation of the valve flaps (leaflets).
Rheumatic fever may also affect:
- The heart muscle, a condition known as myocarditis (inflammation of the heart muscle)
- The outer covering (membrane) of the heart, a condition known as pericarditis (inflammation of the pericardial sac)
Rheumatic fever is the leading cause of valve disease that occurs after birth (acquired valve disease) in the world, but rheumatic fever is not very common in the United States.
Doctors can prevent rheumatic fever by treating strep throat or scarlet fever with medicine (antibiotics).
-
Who is at risk for rheumatic fever?
Children ages 5 to 15 years are at risk for rheumatic fever. They are at greater risk if they have frequent strep throat infections. Rheumatic fever is also more common in children who have a family history of rheumatic heart disease or rheumatic fever. Fewer than 1 out of 300 people who have strep throat also gets rheumatic fever.
Symptoms of Rheumatic Heart Disease
Children with rheumatic heart disease may not have any clear symptoms. Usually, symptoms show up 10 to 20 years after the original illness.
If your child has aortic or mitral valve abnormalities due to rheumatic fever, they may have symptoms, like being short of breath, mainly with activity or when lying down.
Children with myocarditis or pericarditis may have chest pain or swelling.
Your child may also have other effects of rheumatic fever, like joint pain and inflammation.
Heart Center at Seattle Children's
Diagnosing Rheumatic Heart Disease
To diagnose this condition, your doctor will ask about any recent strep infections (like strep throat) or sore throat episodes, examine your child and use a stethoscope to listen to their heart. In children with rheumatic heart disease, doctors can often hear a heart murmur.
During the exam, your child’s doctor will look for signs of inflammation in your child’s joints.
The doctor will ask for details about your child’s symptoms, their health history and your family health history. Your doctor may order a throat culture or a blood test to check for strep throat or signs of a recent strep infection or other blood tests.
Your child will also need tests that provide information about their heart. These may include:
- Chest X-ray
- Echocardiography
- Electrocardiogram
- MRI (magnetic resonance imaging) of the heart
Treating Rheumatic Heart Disease
Children with rheumatic fever need medicine (antibiotics) to fight their strep infection. Your child’s doctor may also prescribe anti-inflammatory medicine to treat joint pain and swelling. They may recommend bed rest for 2 to 12 weeks, based on how serious your child’s illness is. After treatment, your child may still need to take medicine (prophylactic antibiotics) to make sure the infection does not come back.
If your child had rheumatic fever, they need follow-up care with a heart doctor (pediatric cardiologist) to check for long-term heart damage. Pediatric cardiologists at Seattle Children’s Heart Center see children on a regular basis to check for any signs of damage as early as possible. We provide care to prevent problems and to treat any problems that arise.
Once a child gets rheumatic heart disease, they may have to take antibiotics for many years to keep rheumatic fever from returning. Having rheumatic fever again can further damage their heart valves.
If your child has a damaged heart valve that is narrow or leaks enough blood to strain their heart, they may need surgery to repair the valve or replace it with an artificial valve. In some cases, if the valve is too narrow, doctors can use a catheter procedure (balloon valvuloplasty) to try to open the valve without surgery.
Rheumatic Heart Disease at Seattle Children’s
See our statistics and outcomes for mitral and aortic valve repair and replacement.
-
The experts you need are here
- Seattle Children’s team of 40+ pediatric cardiologists diagnose and treat rheumatic heart disease in children of all ages.
- Our pediatric cardiac surgeons perform more than 500 procedures yearly. Each has deep experience operating on children who need a heart valve repaired or replaced.
- We also have a pediatric cardiac anesthesia team and a Cardiac Intensive Care Unit ready to care for children who undergo heart surgery.
- For children with a narrowed heart valve, we are leaders in providing safe and effective catheterization procedures. Typically, these procedures are less painful and have shorter recovery times than surgical treatments.
 “I’m so grateful for the way Seattle Children’s treated us through this entire process. The care Shanae received was amazing, and I wouldn’t change a thing about it.”
“I’m so grateful for the way Seattle Children’s treated us through this entire process. The care Shanae received was amazing, and I wouldn’t change a thing about it.” -
Care from birth through young adulthood
- Our care for rheumatic heart disease starts early. We see babies and children who had rheumatic fever in order to prevent heart damage, watch for signs of damage and treat new concerns before they worsen.
- We match your child’s care to their needs, and we take into account their age, growth and development. Your child’s treatment plan is custom-made for them.
- If your child needs ongoing care as they move into adulthood, we help with this transition. Your team at Seattle Children’s prepares your young adult to take charge of their health and continue getting quality care.
-
Support for your whole family
- We are committed to your child’s overall health and well-being and to helping your child live a full and active life.
- Whatever types of care your child needs, we will help your family through this experience. We will discuss your child’s condition and treatment options in ways you understand and involve you in every decision.
- Our child life specialists know how to help children understand their illnesses and treatments in ways that make sense for their age.
- Seattle Children’s has many resources, from financial to spiritual, to support your child and family and make your child’s journey as smooth as possible.
- Many children and families travel to Seattle Children’s for heart surgery or other care. We help you coordinate travel and housing so you can stay focused on your child.
- Read more about the supportive care we offer.
Contact Us
Contact the Heart Center at 206-987-2515 to request an appointment, a second opinion or more information.
Related Links
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.

