Retinoblastoma
What is retinoblastoma?
Retinoblastoma is a cancer of the eye. It is pronounced reh-tih-no-blas-TOE-muh.
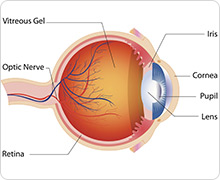
This cancer starts in the lining inside the back of your child’s eye (retina). The retina senses light and sends signals through the optic nerve to the brain.
Cancer in children is very rare. Retinoblastoma accounts for about 3% of childhood cancers. It is most often found in children younger than 2 years.
The cancer may affect 1 eye or both. Most of the time, retinoblastoma is found and treated before it spreads beyond the eye.
What causes retinoblastoma?
Retinoblastoma is caused by a change (mutation) in a gene. Most often, the change affects a gene called RB1. The mutation allows uncontrolled growth of nerve cells in the retina. We do not know why this change happens. It is not because of anything a child or parent does.
Most of the time (about 66%) the mutation happens early in life, starting in 1 cell in 1 eye. This is called sporadic retinoblastoma.
Other children with retinoblastoma are born with a germline mutation, which means the gene mutation is in all the cells in their body. This can happen in 2 different ways.
- A parent passes on the abnormal gene to their child. This is called familial retinoblastoma.
- Very early in pregnancy, the gene changes and the mutation affects all cells in the developing fetus.
Cancer and Blood Disorder Care at Seattle Children's
Symptoms of Retinoblastoma
The most common sign of retinoblastoma is when the black center of the eye (pupil) looks white instead of red when light shines through it. This can be seen during an eye exam or from a camera flash.
These other signs may be caused by retinoblastoma or by another problem. Check with a doctor if your child has any of these:
- Vision problems
- Pain or redness in the eye
- Eyes that look in different directions (crossing inward or wandering outward)
- Clouding of the colored part of the eye (iris) and pupil
Diagnosing Retinoblastoma
-
Exam and tests
To diagnose your child, an eye doctor will:
- Do an exam to check your child’s general health.
- Ask about your child's health and family health history, including whether other family members have had retinoblastoma.
- Check your child’s eyes with a special light and magnifying lens. Eye drops will make the pupil open wider so the doctor can see the back of your child’s eye.
To get more information to diagnose and treat your child, the doctor will:
- Take a more complete look in your child’s eyes after giving them medicine to make them sleep without pain (general anesthesia).
- Take pictures inside your child’s body (imaging studies) to look for tumors or places where cancer can be active. Doctors mostly use MRI (magnetic resonance imaging) of the head and eye sockets to check for retinoblastoma. MRI can make very detailed pictures of the eye and the area around it without using radiation.
-
Staging retinoblastoma
Knowing the stage of your child’s cancer helps us plan the right treatment. The stage of retinoblastoma also affects the chances of saving your child’s vision and their life.
The stage of retinoblastoma is based on:
- The size and location of tumor(s) in the eye
- If the cancer has spread beyond the eye and the location of those cancer cells
Your doctor will talk with you about your child’s stage of retinoblastoma and suggest treatment options after a thorough examination.
-
Genetic counseling and testing
We recommend genetic counseling if your child is diagnosed with retinoblastoma. About 1 in 3 children with retinoblastoma are born with an abnormal gene. This is called germline retinoblastoma.
Children with germline retinoblastoma have a greater chance of:
- Retinoblastoma in both eyes.
- Cancers later in life that affect other parts of the body, such as the bones, muscles, bladder or skin.
- Having a tumor in the pineal gland in their brain. This is rare.
A special blood test can check for the abnormal gene. A person with germline retinoblastoma has a 50% chance in each pregnancy of passing the abnormal gene to their child.
Doctors will check your child more often for signs of retinoblastoma and other cancers if either:
- Genetic testing shows your child has germline retinoblastoma
- There is a family history of retinoblastoma (even without genetic testing to confirm it)
Our Genetic Counseling Clinic can help you understand the pros and cons of genetic testing. Our genetic counselors explain test results and give you information about your child’s condition. Counseling can help you make informed decisions about family planning and your child’s treatment.
Treating Retinoblastoma
“They were able to save Julia’s eye and some of her vision. She no longer has to run with her head turned sideways to watch where she is going.”
We plan your child’s treatment with these goals:
- Save your child’s life
- Save your child’s vision
- Cure their cancer
- Prevent serious side effects, both short-term and long-term
Your child's treatment plan will depend on:
- Whether their retinoblastoma affects 1 eye or both eyes
- The size and location of the tumors in each eye
- If the cancer has spread beyond the eyes
- The likelihood of saving your child’s vision
- How their cancer responds to treatment
- Your child’s age and overall health
- Your family’s preferences for treatment
Treatment options
Many children receive a combination of treatments based on the location and size of the tumors. We offer these treatment options:
-
Intra-arterial chemotherapy
Putting chemotherapy directly into the blood vessel (artery) that feeds the eye and the tumor(s) is called intra-arterial chemotherapy. It also is called super selective intra-optic artery chemotherapy or chemosurgery.
When medicines are put into the artery leading to the eye, doctors can use stronger doses because the medicine has less effect on the rest of the body. The drug is delivered more directly to the tumor, with higher doses in the fluid of the eye. As a result, tumors respond very well and often shrink after this treatment.
Seattle Children’s was 1 of the first hospitals in the country to begin offering intra-arterial chemotherapy. Since 2014, we have provided this treatment more than 100 times. Our doctors are actively involved in national and international research projects to improve this lifesaving and eye-saving treatment.
We offer intra-arterial chemotherapy for children with all stages of retinoblastoma. This treatment is used for children 3 months and older if there are no signs of cancer outside the eye. Because babies younger than 3 months have very small blood vessels, they receive whole-body chemotherapy instead.
Your child will get medicine to make them sleep and not feel pain. Then, doctors:
- Place a very thin, flexible tube (catheter) into a blood vessel on your child’s thigh
- Thread the tube through the blood vessels, through the heart and into the arteries to the head until it reaches the artery that supplies blood to the eye
The medicine your child receives and the number of treatments depend on their cancer.
At Seattle Children’s many children receive intra-arterial chemotherapy to shrink their tumor, followed by freezing or laser treatment.
Your child will receive intra-arterial chemotherapy at our hospital campus in Seattle. Most children spend a night at our Cancer and Blood Disorders Center - Inpatient for careful monitoring.
-
Whole-body (systemic) chemotherapy
Whole-body (systemic) chemotherapy means giving medicines that go throughout your child’s body to kill cancer cells. For retinoblastoma, the medicine usually is injected into your child’s vein. This is called an intravenous (IV) infusion.
Your child’s doctors may suggest whole-body chemotherapy:
- To help shrink a tumor before another type of treatment is used, such as laser or freezing therapy
- To kill any remaining cells after surgery or other treatment
- As the main treatment if retinoblastoma has spread beyond your child’s eyes
Most children receive chemotherapy at our outpatient infusion center on the hospital campus in Seattle as a day procedure.
Children who need more intensive chemotherapy stay in the hospital in our Cancer and Blood Disorders Center - Inpatient (as inpatients).
See more about getting chemotherapy at Seattle Children’s.
-
Intravitreal chemotherapy
Some children need a needle injection of chemotherapy into their eye. This is called intravitreal chemotherapy. It kills cancer cells that are growing within the eye cavity where no blood vessels can reach them. When cells are growing in this space, other forms of chemotherapy through the blood vessels will not reach the cells.
Your child will get medicine to make them sleep and not feel pain. Then, doctors:
- Remove a small amount of fluid from the front of the eye to make space for the medicine
- Inject the chemotherapy into the back of the eye
Most children who get this procedure need multiple treatments over weeks to months.
-
Cryosurgery
Cold treatment (cryosurgery) freezes and destroys cancer cells. Cryotherapy is used for smaller tumors in the front half of the eye. Most children receive chemotherapy first to make the tumor small enough to freeze.
- Your child will get medicine to make them sleep without pain during the treatment.
- Doctors put a small metal probe on the outside of the eye near where the tumor is on the inside.
- The probe is made very cold so that a ball of ice forms over and around the tumor.
- The cancer cells are frozen and thawed several times. This kills them.
- Most likely, your child will get 2 or more treatments, about a month apart.
Cryotherapy is done at our hospital campus in Seattle. Most children are able to leave the hospital the same day as the surgery.
-
Heat treatments (thermotherapy)
Using extreme heat to kill cells is called thermotherapy. Most often, thermotherapy is done with a laser that gives off infrared or green light that heats and kills the tumor cells. This treatment is used for small tumors in the back part of the eye. Most children receive chemotherapy first to make the tumor small enough to treat with a laser.
We will give your child medicine to make them sleep without pain during the treatment. Your child will get 1 or more treatments, about a month apart. Often doctors can treat more than 1 tumor during a single surgery.
Laser therapy is done at our hospital campus in Seattle. Most children do not need to spend a night in the hospital.
-
Surgery
Surgery to remove your child’s eye may be needed if:
- It is not likely that your child’s vision can be saved
- Their tumor is large
- The tumor remains after multiple treatments
- Retinoblastoma comes back in the eye after multiple treatments
If your child needs surgery, doctors will remove their whole eye and part of the optic nerve. This is called enucleation. Surgeons remove the entire eye (not just the tumor) because this is the best way to stop the cancer from spreading.
Your child will get medicine to make them sleep without pain during surgery. After removing the eye, the surgeon sews a plastic implant in your child’s eye socket. The plastic ball is covered and the muscles that move the eye are closed over it. The implant is replaced in about 2 months with a prosthetic eye that can be made to match your child’s remaining eye. Your child’s muscles will move the prosthetic eye somewhat, but it will not move the same way their eye did.
Surgery is done at our hospital campus in Seattle. Most likely, your child will stay in the hospital for 1 or 2 nights before going home.
Learn more about:
-
High-dose chemotherapy and stem cell transplant
If your child’s cancer spreads beyond their eye, they will get high doses of chemotherapy followed by an infusion of their own blood-forming (hematopoietic) stem cells. This is called a stem cell transplant.
High-dose chemotherapy often works better to treat some tumors than standard-dose chemotherapy. But the drugs damage the bone marrow’s ability to make new blood cells. That is why your child needs a transplant of healthy, stored stem cells.
A stem cell transplant using a child’s own cells is called autologous (aw-TAH-luh-gus). Before high-dose chemotherapy, doctors will remove stem cells from your child. The cells are frozen and stored. After chemotherapy is finished, doctors return the stem cells to your child's body through a vein.
We do the transplants here at Seattle Children's, working closely with our partner Fred Hutch. Fred Hutch is one of the largest stem cell transplant centers in the world.
Learn more about our Pediatric Blood and Marrow Transplant Program.
-
Follow-up care
Follow-up care is important after treatment ends — no matter what type of treatment your child had. Your follow-up routine will depend on your child’s cancer and their treatments.
- For children with sporadic retinoblastoma: Follow-up visits happen every 3 months for 18 months after your child’s last treatment. Then visits are every 6 months for 18 months.
- For children with germline retinoblastoma: Follow-up lasts for 5 years from the last active treatment. Your doctor will let you know the schedule that is right for you.
During follow-up visits we will check your child for:
- Ongoing problems from the chemotherapy or eye treatments.
- Any signs that retinoblastoma has returned.
- How their bone marrow, liver and kidneys are working. We will test your child’s blood chemistry and cells.
Your healthcare team will tell you and your child about any risk for other cancers and signs to watch for.
Our Cancer Survivor Program provides long-term follow-up care to help young people stay healthy after being treated for cancer in childhood.
Retinoblastoma at Seattle Children’s
To have the best chance of a cure, your child needs care from a team experienced in treating retinoblastoma in children. Our Brain Tumor Program team collaborates with our Ophthalmology team to treat more children with this eye cancer than any other hospital in the region. We are dedicated to curing retinoblastoma. We are experienced with all treatment options for this disease and do research to improve outcomes.
If you would like an appointment, ask your primary care provider to refer you to Seattle Children’s Cancer and Blood Disorders Center.
If you have a referral or would like a second opinion, contact the center at 206-987-2106.
Providers, see how to refer a patient.
-
The experts you need for comprehensive care
Retinoblastoma treatment requires a dedicated team. At Seattle Children’s our retinoblastoma team includes doctors specially trained to:
- Diagnose and treat cancer in children (pediatric oncologist)
- Treat eye cancer (ocular oncologist)
If your child needs chemotherapy delivered into their eye, they also will get care from a doctor who uses imaging studies to treat diseases (interventional radiologist). Our team works together, and with you, to provide the best care for your child.
Our doctors are active in research groups such as the Global Retinoblastoma Study Group and the International Society of Ocular Oncology. The physician-scientists collaborate to:
- Improve the outlook for children with retinoblastoma
- Find better ways to treat it
- Increase our understanding of the disease and its effect on patients
Your child will benefit from the work of physician-scientists at Fred Hutchinson Cancer Center and UW Medicine, as well as at Seattle Children’s. The National Cancer Institute has named our partnership a comprehensive cancer center.
-
The most advanced therapies
Seattle Children’s provides the most advanced treatments in our region. Our experience helps us recommend the right treatment at the right time to have the best results for your child and your family.
Our treatment options include high-dose cancer-killing medicine delivered directly into the blood vessel that feeds the tumor (intra-arterial chemotherapy or chemosurgery). Seattle Children’s was one of the first hospitals in the country to use this treatment.
We also treat retinoblastoma with chemotherapy, surgery, cryosurgery, heat therapy and stem cell transplants. Our doctors have years of experience with all the available treatment options and will work with you to understand the benefits of each one.
-
Specialists in caring for children with cancer
Our specialty is treating children’s cancer while helping them grow up to be healthy and productive adults.
Our team cares for your whole child. We don’t just treat their disease. As needed, your child will receive care from specialists in nutrition, pain management, pharmacy, palliative care, physical therapy and emotional health. Read more about the supportive care we offer.
Children do not react to illness, injury, pain and medicine in the same way as adults. They need — and deserve — care designed just for them.
We work to make surgery easier on your child and use pain medicines made especially for children. We plan your child’s treatment based on years of experience and the newest research on what works best — and most safely — for children.
-
Support for your whole family
A diagnosis of retinoblastoma can be scary. We take positive steps right away. As soon as we receive your doctor’s referral, we contact you to set up an appointment.
During visits, we take time to explain your child’s condition. We help you fully understand your treatment options and make the choices that are right for your family.
Our doctors, nurses, child life specialists and social workers help your child and your family through the challenges of their illness. We connect you to community resources and support groups.
At Seattle Children's, we work with many children and families from around the Northwest and beyond. Whether you live nearby or far away, we can help with financial counseling, schooling, housing, transportation, interpreter services and spiritual care. Read about our services for patients and families.
Retinoblastoma Team
Professionals from many fields work together to plan and give care to our patients with retinoblastoma.
Pediatric Ophthalmology
-

Jennifer Vincent, COT, Ophthalmic Assistant
-

Austin Zhao, Ophthalmic Assistant
Pediatric Oncologists
Registered Dietitians
-
Mary E Jones Verbovski, MS, RD, CD
-
Garrett Kendall Knecht, RDN, CD
Child Life Specialists
-
Morgan Braun, MS, CCLS, Outpatient Clinic/Infusion Center
-
Alicia Sevilla, MS, CCLS, Outpatient Clinic
Research Coordinators
-
Seehee Park, Clinical Research Associate
-
Grace Rossi, Clinical Research Associate
-
Alicia Sevilla, MS, CCLS, Outpatient Clinic
Contact Us
If you would like an appointment, ask your child’s primary care provider to refer you.
If you have a referral or would like a second opinion, contact the Cancer and Blood Disorders Center at 206-987-2106 or by email.
Providers, see how to refer a patient.
Related Links
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.











Social Workers
Elizabeth Estes, LSWAIC, Brain Tumor Team
Wade Iwata, LICSW, Supervisor, Brain Tumor Team
Back to Top