Moyamoya
 Moyamoya (pronounced MOY-a-MOY-a) is a rare condition that limits blood flow to the brain. It happens when the main blood vessels to the brain (internal carotid arteries) become narrower (stenosis). This makes it harder for oxygen-rich blood to get through. Small blood vessels form to create a new path for blood to flow.
Moyamoya (pronounced MOY-a-MOY-a) is a rare condition that limits blood flow to the brain. It happens when the main blood vessels to the brain (internal carotid arteries) become narrower (stenosis). This makes it harder for oxygen-rich blood to get through. Small blood vessels form to create a new path for blood to flow.
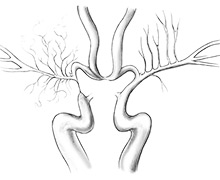
On a picture of the blood vessels in the brain (cerebral angiogram), the new vessels look like a puff of smoke. “Moyamoya” means “hazy puff of smoke” in Japanese. The condition was first reported in Japan.
Moyamoya slows blood flow to the brain and increases the chance of:
- Transient ischemic attack (TIA)
- Stroke
- Seizures
Because of the risk of stroke, moyamoya needs urgent treatment. A stroke or TIA can cause lasting brain damage or death.
If you think your child is having a stroke, call 911.
Some people have moyamoya from very early childhood. Others develop it as they get older. Moyamoya does not get better on its own.
-
Other names for moyamoya
This condition is sometimes called:
- Moyamoya syndrome, when a child has moyamoya along with a condition that increases the risk of moyamoya. These include Down syndrome, and neurofibromatosis (NF) type 1.
- Moyamoya disease, if a child does not have a linked condition but has moyamoya on both sides of their brain
Neurosciences Care at Seattle Children's
Symptoms of Moyamoya
Moyamoya may cause headaches. But often, children have no symptoms until they have a (TIA) or stroke.
Symptoms of a TIA or a stroke from blocked blood flow (ischemic stroke) include:
- Trouble speaking, such as slurring words
- Weakness or numbness on one side of the body
- Sudden vision problems, such as blurred vision
- Trouble walking or balancing
- Seizures
Rarely, children with moyamoya have a stroke from a burst blood vessel (hemorrhagic stroke). This type of stroke may cause:
- Sudden, severe headache
- Trouble walking or balancing
- Trouble staying awake or alert
- Nausea or throwing up (vomiting)
Sometimes, breathing too fast or too deeply (hyperventilating) triggers a TIA or stroke in a child with moyamoya. Crying hard or running may cause your child to breathe too fast.
Diagnosing Moyamoya
Most often, a doctor who specializes in blood flow to the brain diagnoses moyamoya after a child has symptoms of stroke or TIA. Sometimes a brain scan done for another reason finds moyamoya.
To understand your child’s problems and plan treatment, experts in our Pediatric Vascular Neurology Program will ask about your child’s medical history and symptoms and examine your child. As needed, we do to look at the arteries that carry blood to the brain.
If your child might have moyamoya, we will do a complete evaluation to check:
- Balance
- Reflexes
- Motor skills
- Sense of touch
- Memory and thinking
Your child may have 1 or more of these imaging studies:
- scan
- scans of the arteries
- scan
- to map blood vessels in your child’s brain
Some children need other types of imaging to find out how well and how much blood flows to different parts of the brain. Your child’s team will explain which tests your child needs, why and what to expect.
-
Does moyamoya run in families?
Usually, moyamoya affects only 1 person in a family. But in some families, more than 1 person has it. If a child with moyamoya is an identical twin, the other twin should get checked for it. If other family members develop symptoms, they should get checked right away.
-
Risk factors for moyamoya
Certain medical conditions or procedures increase the chance of having moyamoya, such as:
- , also called trisomy 21
- Sickle cell disease
- Neurofibromatosis (NF) type 1
- Noonan syndrome
- Other syndromes caused by problems with
- for a brain tumor
Treating Moyamoya
Doctors treat moyamoya with surgery to bring new blood supply to the brain. Your child’s team at Seattle Children’s will also recommend steps to help reduce stroke risk.
Our Pediatric Vascular Neurology team will talk with you in detail about what they recommend for your child and why.
Surgery Options for Moyamoya
There are 2 main surgeries to improve blood flow in children with moyamoya:
- Indirect revascularization – Surgery that prompts new blood vessels to grow into the brain over time. This surgery is called pial synangiosis (PEE-ul sin-an-JOE-sis) or encephaloduroarteriosynangiosis.
- Direct revascularization - Surgery that sends more blood into blood vessels already in the brain. This procedure is called superficial temporal artery-middle cerebral artery anastomosis, or STA-MCA anastomosis.
Both methods use your child’s superficial temporal artery (STA). Normally, this artery comes up from the neck and goes under the scalp on the side of the head.
We tailor treatment to your child. The neurosurgeon considers your child’s anatomy and health and recommends the best surgery for your child. Whenever possible, we use the indirect method because:
- We believe it is safer for children.
- It does not depend on good blood flow through the middle cerebral artery. Sometimes moyamoya causes narrowing of that artery, which restricts blood flow.
Children who have frequent TIAs or who have a stroke before surgery are at greater risk of having a stroke during surgery or in the next 2 weeks. Overall, this risk is low. To help reduce the risk, we usually wait 4 to 6 weeks after a stroke to do surgery.
Care After Surgery
Most children do very well after surgery for moyamoya. Your child will have pain medicine for their comfort. We will watch your child in the intensive care unit for 1 to 2 days until we are sure they are doing well. Then your child will stay in a regular hospital room for 2 to 3 days. Most children can go home 4 to 5 days after surgery.
Before your child goes home, your child’s team will explain any special care or precautions needed after surgery.
After pial synangiosis, new arteries start growing into the brain. This continues for at least a year. During this time, your child may have headaches or TIAs. Over time, this should improve. We ask you to keep track of your child’s symptoms, so we can talk about them at follow-up visits and give your child any tests or treatments they need.
As part of follow-up care, we check to see if moyamoya is developing on the other side of your child’s brain. If it does, we will treat it.
We tailor the follow-up schedule to your child. Here is what usually happens:
- About 2 weeks after surgery, the neurosurgery team will see your child for a follow-up visit. We check your child’s healing and remove their stitches.
- In about 3 months, a and a will see your child for a follow-up visit. Your child will have an scan. These tests check blood flow in the affected areas of your child’s brain.
- Each year, your child will have a brain scan.
-
Lowering the risk of stroke
Even after surgery, your child will have a higher risk of stroke than most children. Some blood vessels in your child’s brain will not be as big as normal.
We will teach you – and your child, when they are old enough – how to lessen the risk of stroke, such as:
- Take a low dose of aspirin each day to prevent blood clots that could block small arteries.
- Avoid medicines that constrict the blood vessels, unless recommended by a doctor who knows about moyamoya and your child’s health history. These include medicines for migraine headaches.
- Drink water and other fluids each day to keep your child’s blood volume and blood pressure high enough for good blood flow.
- Use caution if taking medicines that increase the risk of blood clots, such as birth control pills.
- Protect the brain and its arteries with a helmet during activities like biking, skiing or skateboarding.
- Avoid strenuous activity in the months right after surgery. Talk to your child’s team about the right level of activity for your child.
Ongoing Care
Seattle Children’s provides follow-up care to:
- Monitor your child’s health
- Prevent complications
- Manage symptoms or other health problems
- Improve your child’s quality of life
Ongoing care will depend on your child’s needs. For example, if reduced blood flow damaged your child’s brain, they may benefit from:
Our team is experienced in helping children return to school and other important activities after brain surgery or treatment for stroke. We also work with you to find resources in your community.
-
Transition to adult care
As your child gets older, we prepare them to take on a greater role in their own care. When your child is ready, we connect them with experts who can meet their adult healthcare needs.
We work closely with the neurosurgeons at Harborview Medical Center who treat moyamoya. Many of the doctors who treat moyamoya at Seattle Children’s also treat adults with moyamoya at Harborview.
Why choose Seattle Children’s for your child's moyamoya care?
Because moyamoya is very rare, most doctors never see a child with this condition. Each year, Seattle Children’s treats many patients with moyamoya, from babies to young adults. Experts in our Pediatric Vascular Neurology Program work as a team to care for your child — from diagnosis to surgery to long-term follow-up. We also provide second opinions.
The program director, Dr. Catherine Amlie-Lefond, is a pediatric and national leader in this field. Seattle Children’s is the only children’s hospital in our region with a program focused on children who have problems that affect the brain’s blood flow and vessels. Our region includes Washington, Alaska, Montana and Idaho (WAMI).
Children come here from across the country for surgery called pial synangiosis (PEE-ul sin-an-JOE-sis) to improve blood flow to their brain and reduce the risk of stroke. Dr. Richard G. Ellenbogen performs many of these operations every year on babies, children and teens. We have some of the best outcomes in the nation for .
Each child’s case is unique. Pediatric experts in Neurosurgery and Neurology will care for your child. Based on your child’s needs, your team may include specialists from Interventional Radiology, Neuropsychology, Social Work and Rehabilitation Medicine.
If moyamoya causes a stroke, we have the expertise to respond quickly for the best possible outcome. As needed, we provide rehabilitation for your child’s recovery. If your child has another condition linked with moyamoya, team members work together and with you to develop the best treatment plan to take care of all your child’s health needs.
-
Care from birth through young adulthood
Our Pediatric Vascular Neurology Program coordinates care for moyamoya patients from birth through young adulthood. We are experts in pediatrics and the ways cerebrovascular conditions are different in children than in adults.
We see babies, children and teens who:
- Have symptoms but have not been diagnosed
- Have been diagnosed and need surgery
- Had surgery somewhere else for moyamoya and want to change doctors or need a second opinion about the best treatment
We take care of your child over the long term – not only in the weeks and months before and after surgery, but for years to come. During follow-up care, we keep a watch on your child’s health to help them have the best quality of life.
As your child gets older, we prepare them to take on a greater role in their own care. When your child becomes an adult, we help them transition to care at Harborview Medical Center.
-
Support for your whole family
- During visits, we take time to explain your child’s condition. We help you fully understand your treatment options, so you can make the choices that are right for your family.
- Our doctors, nurses, child life specialists and social workers help your child and your family through the challenges of their condition. We connect you to community resources and support groups.
- As your child grows, we meet their changing needs, whether they are a young child going back to school after brain surgery or a teen taking on more responsibility for their health.
- At Seattle Children’s, we work with children and families from around the Northwest and beyond. We can help with financial counseling, schooling, housing, transportation, interpreter services and spiritual care. Read about our services for patients and families.
Contact Us
- If you would like an appointment, ask your child’s primary care provider to refer you.
- If you have a referral, call 206-987-2016 to make an appointment.
- Providers, see how to refer a patient.
- If you have any questions, please contact us at 206-987-2016or 844-935-3467 (toll free).
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.

