Crouzon Syndrome
What is Crouzon syndrome?
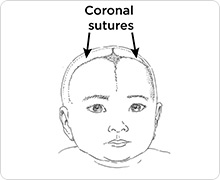
Crouzon syndrome is a rare genetic form of craniosynostosis — the early closing of 1 or more of the soft, fibrous seams (sutures) between the skull bones. Crouzon is pronounced kroo-ZAHN.
Because some of the bones of the skull and the face fuse early, the bones cannot grow normally. In particular, the middle of the face and eye sockets are not formed correctly.
This often leads to breathing problems as your child grows. It also affects the shape of their head, how their face looks and how teeth in the upper and lower jaws line up.
People with Crouzon syndrome usually have normal intelligence.
The syndrome is named after the French doctor who first described it. Crouzon syndrome is estimated to happen in 1 out of every 60,000 newborns.
Children with Crouzon syndrome need coordinated care by providers from many areas of healthcare. At Seattle Children’s Craniofacial Center, our team of experts covers 19 different specialties.
-
What causes Crouzon syndrome?
Crouzon syndrome is caused by a change (variant) in a that is important in forming bone. Usually the change affects the FGFR2 gene (fibroblast growth factor receptor 2). A form of Crouzon syndrome that affects the skin is caused by a mutation in the FGFR3 gene. That form is called Crouzon syndrome with .
Often the condition is caused by a new genetic change that was not inherited from the mother or father. Other times, a parent passes the gene variant to a child.
Seattle Children's Craniofacial Center
Symptoms of Crouzon Syndrome
The head and face of a child with Crouzon syndrome look different because of craniosynostosis —the early closing of the soft, fibrous seams between the skull bones (sutures).
 Drawn by Raymond Sze
Drawn by Raymond Sze
Crouzon syndrome often affects the coronal sutures that go over the top of the head from ear to ear. But other sutures also may close (fuse) early.
Usually, these sutures let the skull get bigger as the brain grows. During childhood, the sutures slowly grow together to fully connect the skull bones. The different sutures close at different times. The process continues until adulthood.
In Crouzon syndrome, the early closing of a suture usually happens before birth. But it can happen later, when a child is 2 or 3 years old, depending on the sutures affected.
If a suture closes early, it changes the shape of the head and reduces room for the growing brain. This can increase pressure inside your child’s skull.
-
Symptoms affecting the face and head
The facial features of babies with Crouzon syndrome vary widely.
You may see these differences in your child:
- A taller head shape that is narrow from front to back.
- Wide-set eyes that seem to stick out because their eye sockets are shallow.
- Eyes that do not line up.
- A small, pointed nose. This often causes breathing problems.
- Smaller middle of the face (midface) compared to the rest of the face.
-
Changes to the head as your child grows
The differences in your child’s face and head will likely become more noticeable as they grow.
Over time their upper jaw may look smaller and the lower jaw may stick out (underbite). This is because bones in the middle of their face grow slower than other parts of their head.
The roof of their mouth (palate) may be narrow. This crowds their upper teeth and positions them behind the lower jaw during chewing.
Headaches and vision changes in a child 2 to 3 years old may be a sign that 1 of the sutures in the skull is closing too soon. This is called late-onset craniosynostosis.
-
Changes affecting other parts of the body
Many children with Crouzon syndrome have hearing loss. Some babies are born without ear canals.
Unlike most other craniosynostosis syndromes, Crouzon syndrome rarely involves the hands and feet. But it may cause problems in the neck (cervical spine). Less often, there may be small differences in the elbow, bones and muscles or internal organs.
About 5% of people with Crouzon syndrome develop a skin condition called acanthosis nigricans. They have patches of darker, thicker (velvety feeling) skin. The patches may be on their neck and eyelids and around their mouth and other areas of thin skin.
Diagnosing Crouzon Syndrome
To diagnose this condition, your doctor will examine your child’s skull carefully. The shape will help the doctor tell whether any sutures have closed too soon.
Your child’s facial features will help the doctor decide if they have Crouzon syndrome or another condition.
A CT (computed tomography) scan of your child’s head can give the doctor more information and help us plan the best treatment for your child.
-
Genetic counseling and testing
Our Craniofacial Genetics Clinic helps identify conditions caused by changes in genes. Our geneticists and genetic counselors can advise you about the pros and cons of genetic testing. They explain test results and your chance of having a child with Crouzon syndrome in a future pregnancy.
Our genetic counselor also will give you information about your child’s condition. Counseling can help you make informed decisions about family planning and your child’s treatment.
Our genetic counselors also advise people with Crouzon syndrome about their chance of having a child with the syndrome.
- A person with Crouzon syndrome has a 50% chance in each pregnancy of passing down the gene variant that causes the condition.
Treating Crouzon Syndrome
There is no single care plan for Crouzon syndrome. The treatments and timing we recommend depend on how your child is affected by the syndrome.
Our goal is to minimize the number of steps in the treatment plan by improving the outcome of each step.
-
Easing breathing
Making sure your child is breathing well is an immediate priority. Differences in the bones in the jaw or midface or an abnormal windpipe can make it hard to breathe.
For children with severe breathing difficulties, they may need a tube inserted in their windpipe (tracheostomy) soon after birth.
Later, your child will likely have surgery to reposition their jaw and face bones to help with breathing and other problems.
Sometimes children have trouble breathing while they sleep (obstructive sleep apnea). Over time, this may lead to problems with how the heart and lungs work. It also can contribute to problems with learning and behavior.
We will ask questions during clinic visits to assess whether this may be a problem. To better understand their breathing patterns, we may monitor your child overnight in our sleep lab (PDF) (Arabic) (Simplified Chinese) (Somali) (Spanish) (Vietnamese).
-
A healthy brain with room to grow
Most children with Crouzon syndrome will need surgery to expand and reshape their skull.
Most children with this condition have early closure of a suture in their skull (craniosynostosis) at birth or in infancy. In other children, problems with fused skull bones happen later. In mild cases of Crouzon, children may not have early closure of their skull bones.
We check your child regularly and recommend surgery as needed. A craniofacial plastic surgeon and neurosurgeon work as a team in the operating room to protect your child’s brain and achieve the best results.
- Most children who need surgery to expand their skull will have a procedure called fronto-orbital advancement.
- Less often, we recommend posterior cranial vault distraction.
- In severe cases, a child will need a procedure called monobloc frontofacial advancement to reposition the forehead and midface.
The procedure and timing of surgery will depend on which sutures have closed too soon and how many are affected. If more than 1 suture is affected, your baby may need surgery in their first months of life. Some children who have early surgery will need a follow-up operation, but this is not common.
Some children with Crouzon syndrome need surgery because their brain is pressing on the base of their skull. This happens if a child has a Chiari malformation (abnormality in the back of the brain).
Checking fluid build-up and pressure in the skull
About 3 out of every 10 children with Crouzon syndrome have extra fluid in the skull (hydrocephalus). Symptoms in infants include:
- A bulging soft spot (anterior fontanelle)
- Rapidly increasing head size
- Acting cranky or sluggish
Older children may have:
- Headaches (worse in the morning)
- Vomiting
- Poor vision
- Declining school performance.
Your child’s team will check for signs of fluid build-up and increased pressure in the skull. These problems can happen during infancy or as your child grows.
- If fluid collects in your child’s brain, they may need a tube (shunt) inserted to drain away extra fluid. The fluid drains into another part of the body, where it can be absorbed.
- At regular checkups, we ask about warning signs of increased pressure. If there are concerns, your child may have imaging scans or a special eye exam to check for swelling at the back of the eye. Warning signs include headaches or problems with eyesight.
-
Midface surgery to improve breathing
In many children with Crouzon syndrome, their nose is small and the bones in the middle of the face (midface) do not grow right. Their eyes are not protected because their cheekbones are too small. They may have trouble breathing, especially while they sleep.
For some children, surgery to remove adenoids or lymphoid tissue in the back of the nose (adenoidectomy) will improve their breathing.
Most children need Le Fort III midface advancement surgery combined with distraction osteogenesis to bring forward the jaw and other bones of the middle face.
Le Fort III midface advancement with distraction
Le Fort III midface advancement and distraction enlarges your child’s airway and helps their jaws fit together better. It also creates larger cheekbones to protect their eyes.
Seattle Children’s pioneered midface distraction in the Northwest. We perform this surgery more often than most centers in the country. Our method results in less scarring and a shorter distraction time.

BEFORE (Above, left): The middle of this girl’s face did not grow well because of Crouzon syndrome. This caused severe breathing problems.
DISTRACTION (Above, center): During surgery to reposition her face bones, a device called a distractor was attached. While she recovered at home, the distractor was adjusted to move the bones slowly apart. New bone grew to fill in the gaps.
AFTER (Above, right): After the procedure, the child has a larger airway so she can breathe during sleep. Her cheekbones are larger and her teeth fit together better.
Timing of surgery depends on your child’s needs
The timing of midface advancement is based on whether your child has:
- Chewing and speech difficulties caused by the jaws not aligning
- The need for eye protection
- Breathing problems while asleep
Most often, children with sleep apnea have the surgery at 7 to 9 years old to improve breathing. If your child has severe breathing problems, they may need a Le Fort III distraction as early as 3 years old.
-
Protecting eyesight
An eye doctor (ophthalmologist) will check your child regularly for problems with their eyesight.
- If your child has very shallow eye sockets, their eyes may stick out (proptosis) and be at greater risk of injury.
- Your child’s eyes may not align in the right way because of the position or shape of the eye sockets. This can affect their vision.
- Increased pressure inside the skull can also cause problems with your child’s eyesight.
- Some children with Crouzon syndrome cannot close their eyes completely. That can irritate the covering on the front of their eyes (corneas). The condition is called keratitis. To avoid harm to their vision, your child may need surgery before they are 2.
The best procedure to protect their eyes depends on your child:
- Le Fort III midface advancement to move the middle part of the face forward. It creates larger cheekbones that protect the eyes. This is done at age 8 to 10.
- Fronto-orbital advancement to bring the forehead and upper eye sockets forward to help protect the eyes. This surgery also may be done if your child cannot close their eyes completely.
- Monobloc frontofacial advancement to expand the skull and advance the midface. This is not used often, but is the best choice for young children whose cheekbones and brow bones are behind their eyes.
-
Dental care and bite alignment
Good mouth care (oral hygiene) is important for all children, but especially those with craniofacial disorders.
A pediatric dentist will check your child’s general dental health and look to see if their teeth are too crowded. As your child grows, a craniofacial team orthodontist will check how your child’s upper and lower teeth fit together (occlusion).
Learn more about craniofacial orthodontics.
Your child may need:
- Upper teeth removed to relieve crowding because of their small upper jaw.
- Orthodontic braces to expand the roof of their mouth (palate) and align their teeth.
- Braces or appliances to put the teeth in the best position before jaw surgery.
- Braces to hold the teeth in the correct position for at least 6 months after jaw surgery.
- Surgery to move the upper jaw forward (Le Fort I maxillary advancement) if your child’s teeth do not fit together well when their face bones have finished growing. Usually, this happens at 16 years for a female and 18 years for a male. Many children with Crouzon syndrome need this adjustment as teenagers even though their upper jaw was enlarged as a result of Le Fort III midface advancement when they were younger.
-
Managing hearing and speech problems
Many children with Crouzon syndrome have hearing loss.
Usually your baby’s hearing is screened in the hospital soon after birth or within a few days. If problems are found, we do further testing.
As your child grows, they will have a variety of hearing tests based on their hearing status and ear health. A specialist trained to test hearing in infants and children (audiologist) will perform the tests.
Our ear, nose and throat specialist (otolaryngologist) and audiologist will talk with you and your child about hearing management, such as:
- Whether hearing aids are needed
- The best place to sit in the classroom when your child reaches school age
Hearing problems can lead to speech difficulties. Your child may have problems with speech if the roof of their mouth or the inside of their nose has an unusual shape or size.
If needed, a speech and language pathologist (SLP) will evaluate your child and recommend speech therapy or other treatment.
Crouzon Syndrome at Seattle Children’s
Many families have never heard of craniosynostosis before their child is born with Crouzon syndrome. Each year we care for hundreds of children with craniosynostosis, including rare syndromes like Crouzon. Our team has more experience caring for children with craniosynostosis than any other center in the United States.
Many of our patients are babies who are newly diagnosed. We also work with children who received their initial treatment at another hospital.
Please call the Craniofacial Center at 206-987-2208 for more information, a second opinion or to make an appointment.
-
Your child is in the hands of experts
Every year we care for more than 150 children with craniosynostosis syndromes, including Crouzon.
Our experience with craniofacial conditions helps us find problems early and take steps to prevent or treat them. We watch carefully for problems that may develop with your child’s breathing, feeding, vision, hearing, speech and development.
Our experience with this rare condition helps us to continually improve our care. We can recommend the right treatment at the right time to have the best results for your child and your family.
-
Better results with fewer surgeries
Seattle Children’s surgeons are experienced in the complex surgery children with Crouzon syndrome may need, whether to expand their skull, lengthen their jaw bone or reposition their face bones.
Our approach helps children with Crouzon syndrome get the maximum benefit from surgeries they have early in childhood. As a result, later in life, some surgeries are either not needed or are less extensive.
- Often our treatment involves 2 types of surgery: cutting bone in the operating room, followed by distraction osteogenesis to grow a longer bone. A device called a distractor is used for several weeks after leaving the hospital. Cutting a bone and then stretching it with a distractor lets us make bigger corrections in bone position.
- 3-D imaging and powerful software help us predict future growth. Our surgery and orthodontic corrections take into account continued growth of your child’s bones. When your child is finished growing, their bones are in the desired position.
-
Specialists to cover all your child’s needs
Our center has experts in every field your child might need. These 50 specialists work as a team to diagnose and care for our patients.
Our team meets weekly to discuss children with complex needs and decide on the best care plan for each child. We work together, and with you and your family doctor, to manage your child’s personalized care.
A craniofacial pediatrician, nurse and social worker will work closely with your family. They help coordinate care and make sure all your questions are answered.
Your child’s craniofacial pediatrician guides your child’s treatment and decides if other specialists are needed. Your child’s team may include a pediatric neurosurgeon, craniofacial plastic surgeon, oral-maxillofacial surgeon, orthodontist, ophthalmologist, otolaryngologist, nurse, social worker and other experts in our center.
We care for care for your child’s physical, emotional and comfort needs. Read more about the supportive care we offer.
-
We support your whole family
A diagnosis of Crouzon syndrome can be scary. We take time to explain your child’s condition. We help you fully understand your treatment options and make the choices that are right for your family.
As your child gets older, we include them in decisions about their medical care. Our child life specialists and social workers support your child and family through the challenges of this condition. We also connect you to community resources and support groups.
-
Research to improve care
Our team has created a clinical care pathway for craniosynostosis. It guides our treatment of related syndromes like Crouzon. It is based on the research evidence about what is most effective and outlines treatment from diagnosis onward.
We receive more research funding from the National Institutes of Health (NIH) than any other craniofacial center in the United States.
Our research is helping us to:
- Learn more about the genetic causes of craniosynostosis
- Understand how the condition affects learning and behavior
- Build a library of 3-D images to better measure the results of surgery and improve treatments
Learn about craniosynostosis research at Seattle Children’s.
Contact Us
Contact the Craniofacial Center at 206-987-2208 for an appointment, a second opinion or more information.
Providers, see how to refer a patient.
